Diverticulitis
Introduction
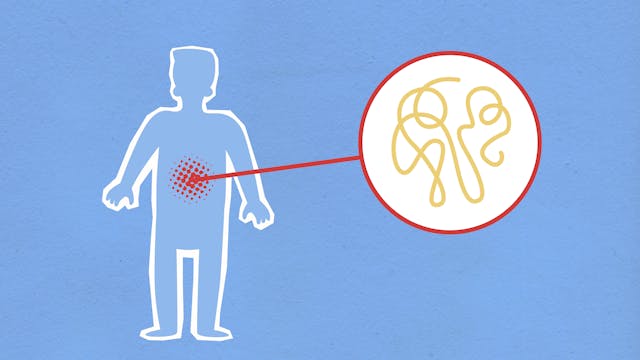
Diverticulitis is a medical condition characterized by the inflammation or infection of diverticula, which are small, bulging pouches that can form in the lining of the digestive system. These pouches are most commonly found in the lower part of the large intestine (colon). Diverticulitis can cause severe abdominal pain, fever, nausea, and a significant change in bowel habits.
This comprehensive guide aims to provide detailed information about diverticulitis, including its causes, risk factors, symptoms, diagnosis, treatment options, lifestyle management, and prevention strategies.
Understanding Diverticulitis
What is Diverticulitis?
Diverticulitis occurs when one or more diverticula in the digestive tract become inflamed or infected. The condition can range from mild to severe and may lead to complications if not properly treated. Diverticula themselves are usually harmless and often go unnoticed; however, when they become inflamed, they can cause significant discomfort and health issues.
Difference Between Diverticulosis and Diverticulitis
Diverticulosis: This is the presence of diverticula in the colon. It is generally asymptomatic and is often discovered incidentally during routine examinations or imaging tests for other conditions.
Diverticulitis: This occurs when the diverticula become inflamed or infected, leading to symptoms such as abdominal pain and fever.
Anatomy and Physiology of the Colon
The colon, or large intestine, is an essential part of the digestive system responsible for absorbing water and electrolytes from indigestible food matter and forming solid waste (stool) for excretion. Diverticula form when weak spots in the colon wall give way under pressure, creating pouches that protrude through the muscular layer of the intestinal wall.
Causes and Risk Factors
Causes of Diverticulitis
The exact cause of diverticulitis is not completely understood, but several factors may contribute to the development of the condition:
Increased Pressure in the Colon: Chronic increased pressure in the colon can lead to the formation of diverticula. When these diverticula become obstructed by stool or undigested food particles, they can become inflamed or infected.
Diet: A low-fiber diet is commonly associated with diverticulitis. Fiber helps soften stool and reduce the pressure required to move it through the colon.
Bacterial Infection: The obstruction of a diverticulum can lead to bacterial overgrowth and infection.
Inflammation: Inflammation of the diverticula can occur due to various factors, including dietary habits and genetic predisposition.
Risk Factors for Diverticulitis
Several risk factors can increase the likelihood of developing diverticulitis:
Age: The risk of diverticulitis increases with age, particularly after the age of 40.
Diet: A diet low in fiber and high in red meat and processed foods can increase the risk.
Lack of Physical Activity: Sedentary lifestyles are associated with a higher risk of diverticulitis.
Obesity: Overweight and obese individuals are at a higher risk.
Smoking: Smokers have a higher likelihood of developing diverticulitis compared to non-smokers.
Certain Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), steroids, and opioids may increase the risk of diverticulitis.
Genetics: A family history of diverticulitis can predispose individuals to the condition.
Symptoms
Common Symptoms
Diverticulitis can present with a variety of symptoms, which may range from mild to severe. Common symptoms include:
Abdominal Pain: Typically, the pain is located in the lower left side of the abdomen. It may be constant and persistent.
Fever: A low-grade fever often accompanies the inflammation.
Nausea and Vomiting: These symptoms can occur due to the gastrointestinal upset caused by the condition.
Changes in Bowel Habits: Diarrhea or constipation can occur. Some individuals may experience alternating bouts of both.
Bloating and Gas: These symptoms are due to the inflammation and obstruction in the colon.
Tenderness: The abdomen may feel tender to the touch.
Severe Symptoms and Complications
In severe cases, diverticulitis can lead to complications, which may present with more serious symptoms:
Abscess: A localized collection of pus can form in the infected diverticula.
Fistula: An abnormal connection can develop between the colon and adjacent organs, such as the bladder or vagina.
Perforation: A hole in the colon wall can occur, leading to peritonitis, a serious abdominal infection.
Intestinal Obstruction: Blockage of the intestine can result from severe inflammation or scarring.
Bleeding: Although less common, bleeding can occur from a ruptured diverticulum.
Diagnosis
Medical History and Physical Examination
Diagnosis of diverticulitis typically begins with a thorough medical history and physical examination. The healthcare provider will inquire about the patient’s symptoms, dietary habits, medical history, and family history of gastrointestinal diseases. During the physical examination, the abdomen will be palpated to assess for tenderness and other signs of inflammation.
Diagnostic Tests
Several diagnostic tests can help confirm the diagnosis of diverticulitis and assess its severity:
Blood Tests: Elevated white blood cell count may indicate infection or inflammation.
Stool Tests: These tests can help rule out other causes of gastrointestinal symptoms, such as infections.
CT Scan: A computed tomography (CT) scan of the abdomen and pelvis is the preferred imaging test for diagnosing diverticulitis. It can show inflamed or infected diverticula, abscesses, and other complications.
Ultrasound: An abdominal ultrasound can sometimes be used to detect diverticulitis, especially in pregnant women to avoid radiation exposure.
X-ray: Abdominal X-rays may be used to detect complications such as perforation or obstruction.
Colonoscopy: Although not typically used for diagnosing acute diverticulitis due to the risk of perforation, a colonoscopy may be recommended after the inflammation has subsided to rule out other conditions such as colorectal cancer.
Treatment
Mild Diverticulitis
For mild cases of diverticulitis, treatment typically involves:
Dietary Changes: A clear liquid diet is often recommended initially to allow the colon to heal. Gradual reintroduction of solid foods, starting with low-fiber options, follows as symptoms improve.
Antibiotics: Oral antibiotics may be prescribed to treat the infection. Commonly used antibiotics include metronidazole, ciprofloxacin, and amoxicillin-clavulanate.
Pain Relief: Over-the-counter pain relievers such as acetaminophen are preferred. NSAIDs like ibuprofen are generally avoided due to their potential to exacerbate gastrointestinal symptoms.
Rest: Adequate rest is crucial to allow the body to recover.
Severe Diverticulitis
Severe or complicated cases of diverticulitis may require more intensive treatment, including:
Hospitalization: Patients with severe symptoms, high fever, or complications may need to be hospitalized for closer monitoring and treatment.
Intravenous (IV) Antibiotics: Stronger antibiotics administered intravenously are often necessary for severe infections.
IV Fluids: To maintain hydration and electrolyte balance, IV fluids may be given.
Drainage of Abscess: If an abscess has formed, it may need to be drained using a needle guided by CT or ultrasound.
Surgery: Surgery may be required for patients with recurrent diverticulitis, fistulas, obstructions, or perforations. Surgical options include:
Bowel Resection: Removing the affected portion of the colon.
Primary Anastomosis: Reconnecting the healthy parts of the colon after resection.
Colostomy: Creating an opening (stoma) in the abdominal wall to divert waste, which may be temporary or permanent.
Lifestyle Management and Prevention
Dietary Recommendations
High-Fiber Diet: Increasing dietary fiber intake can help prevent the formation of diverticula and reduce the risk of diverticulitis. Foods rich in fiber include fruits, vegetables, whole grains, and legumes.
Hydration: Drinking plenty of water helps soften stool and reduce pressure in the colon.
Avoiding Trigger Foods: Some individuals may find relief by avoiding foods that seem to trigger their symptoms, such as nuts, seeds, and popcorn, though recent research suggests these foods may not need to be avoided universally.
Gradual Introduction of Fiber: For those not used to a high-fiber diet, gradually increasing fiber intake can help prevent gastrointestinal discomfort.
Physical Activity
Regular physical activity is beneficial for overall digestive health and can help reduce the risk of diverticulitis. Aim for at least 30 minutes of moderate exercise most days of the week.
Weight Management
Maintaining a healthy weight can reduce the risk of developing diverticulitis. Weight loss strategies should include a balanced diet and regular exercise.
Avoiding Smoking and Excessive Alcohol Consumption
Quitting smoking and limiting alcohol intake can improve overall health and reduce the risk of diverticulitis.
Living with Diverticulitis
Coping with Symptoms
Pain Management: Using prescribed pain relievers and applying heat pads to the abdomen can help manage pain.
Stress Management: Stress can exacerbate symptoms, so incorporating relaxation techniques such as yoga, meditation, and deep breathing exercises can be beneficial.
Monitoring and Follow-up
Regular follow-up appointments with a healthcare provider are important for monitoring the condition and preventing recurrences. Discuss any new or worsening symptoms with your provider promptly.
Educating Yourself and Others
Understanding diverticulitis and staying informed about new research and treatment options can empower individuals to manage their condition effectively. Support groups and educational resources can provide additional support and information.
Conclusion
Diverticulitis is a common digestive condition that can cause significant discomfort and complications if not properly managed. Understanding the causes, symptoms, and treatment options is essential for effective management and prevention. By making lifestyle changes such as adopting a high-fiber diet, staying physically active, and maintaining a healthy weight, individuals can reduce their risk of developing diverticulitis and improve their overall digestive health.
Early diagnosis and appropriate treatment are crucial in managing diverticulitis and preventing serious complications. Regular medical check-ups and open communication with healthcare providers are key components of effective management. With the right strategies and support, individuals with diverticulitis can lead healthy, fulfilling lives.